Iron-deficiency anaemia is the most common type of anaemia. It happens when you do not have enough iron in your body. Iron deficiency is usually nutritional or due to blood loss or poor absorption of iron. Pregnancy and childbirth consume a great deal of iron and thus can result in pregnancy-related anaemia. People who have had gastric bypass surgery for weight loss or other reasons may also be iron deficient due to poor absorption.
Vitamin-deficiency anaemia may result from low levels of vitamin B12 or folate (folic acid), usually due to poor dietary intake.
Pernicious anaemia is a condition in which vitamin B12 cannot be absorbed in the gastrointestinal tract.
Anaemia and Pregnancy – Learn about the risk factors and symptoms of anaemia during pregnancy.
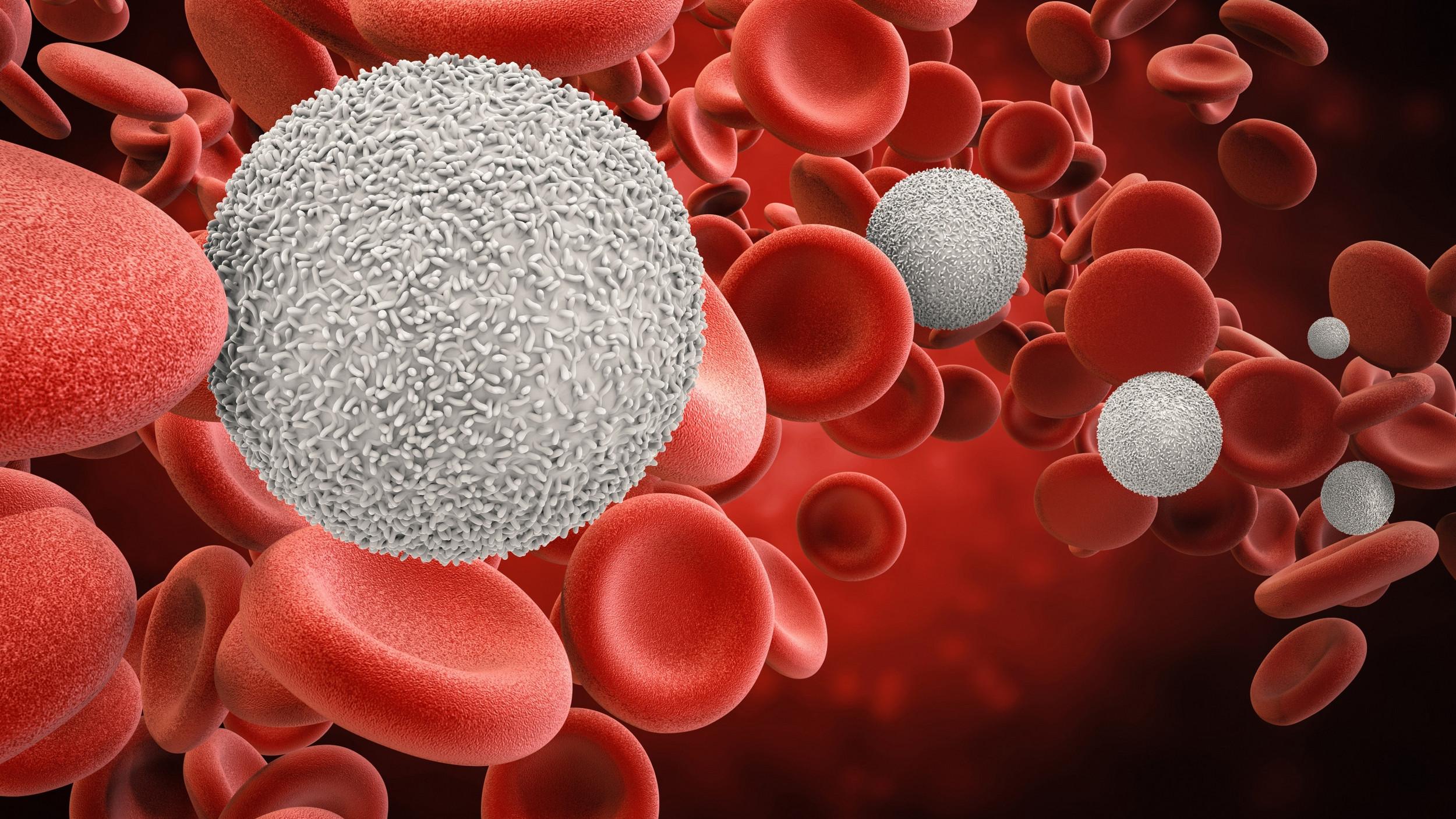
Aplastic anaemia is a rare bone marrow failure disorder in which the bone marrow stops making enough blood cells (red blood cells, white blood cells, and platelets). This occurs as a result of destruction or deficiency of blood-forming stem cells in your bone marrow, in particular when the body’s own immune system attacks the stem cells. Viral infections, ionizing radiation, and exposure to toxic chemicals or drugs can also result in aplastic anaemia.
Haemolytic anemia occurs when red blood cells are broken up in the bloodstream or in the spleen. Haemolytic anemia may be due to mechanical causes (leaky heart valves or aneurysms), infections, autoimmune disorders, or congenital abnormalities in the red blood cell. Inherited abnormalities may affect the haemoglobin or the red blood cell structure or function. The treatment will depend on the cause.
Sickle cell anaemia is an inherited haemolytic anaemia in which the haemoglobin protein is abnormal, causing the red blood cells to be
rigid and clog the circulation because they are unable to flow through small blood vessels.
Anaemia caused by other diseases – Some diseases can affect the body’s ability to make red blood cells. For example, some patients with kidney disease develop anaemia because the kidneys are not making enough of the hormone erythropoietin to signal the bone marrow to make new or more red blood cells. Chemotherapy used to treat various cancers often impairs the body’s ability to make new red blood cells, and anaemia often results from this treatment.